Untangling the Threads: Power, Politics and the Pill
Leave Unanswered Questions for Women's Health
By Mary Elizabeth Fratini
Untangling the nuances of medical data is never easy (even when pharmaceutical companies do make it public) but interpreting the most recent studies on the long-term use of oral contraceptives is even more complex given the long (and lingering) history of politics trumping science in women's public health.
The introduction of hormonal contraception (the Pill) in 1960 fundamentally altered the relationship between a woman's body and the rest of her life. As one woman reminisced in a PBS documentary, law firms were suddenly free to hire women as partners without worrying they would become pregnant in the middle of an important case. Or as another put it, you could be sexual, you could be a good girl, and you could still have a future.
Birth of The Pill
Prior to the Pill, the only available contraceptive methods were condoms, diaphragms and in some cases radical hysterectomies. The U.S. was at the height of the baby boom - most women were married by 19 and more than half of them were pregnant within the first year. While Margaret Sanger's long crusade for women's access to family planning information had made progress, more than 30 states still had Comstock laws on the books based on a 19th century federal law defining contraceptives as obscene and illicit; some outlawed the use of birth control altogether, including Connecticut. Dr. Richard Hauskenecht, a Connecticut physician during the 1950s and '60, recalled the use of hysterectomies for birth control: "We did them early after delivery," he told PBS. "And doing a vaginal hysterectomy on somebody who's had three or four kids, six weeks postpartum, you got two choices: you either got to be faster than hell, or you'd better get the blood bank cranked up because the blood loss will be astonishing. It was prehistoric, absolutely prehistoric."
Within five years of its final approval by the FDA for use as a contraceptive, more than six million American women were taking the Pill, though it met resistance in the African American community. Sterilization abuse of black women in the South had been so widespread in the early half of the 20th century that it was known as a "Mississippi appendectomy" and many communities first saw the Pill as a hidden attempt at eugenics.
Before the end of the decade, however, women were complaining of the same side effects documented in early trials of the Pill in Puerto Rico in 1956, including strokes. In 1970, Congress held hearings on the safety of the Pill that were interrupted by women protesting their exclusion from testifying. Journalist Barbara Seaman, whose 1969 book The Doctors' Case Against the Pill exposed the safety risks of the first generation of pills, called the protests the "Boston Tea Party of the women's health movement."
Today's Pill, Tomorrow's Health
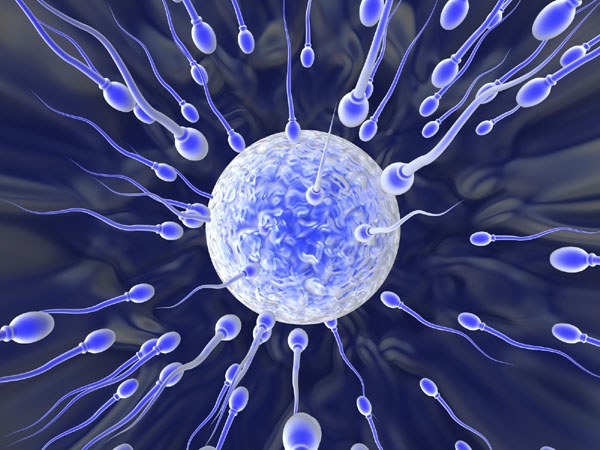
Today, contraception encompasses behavioral, over the counter, prescription and permanent methods, but one-third of American women opt for hormonal contraception. More than 10 million American women use the Pill daily according to the Association of Reproductive Healthcare Providers (ARHP). There is also "the ring", "the patch", "the shot" and "the implant" and at least one brand of IUD, all of which release either a single hormone or combination of hormones over a predetermined period of time; they prevent pregnancy by preventing ovulation, altering the lining of the uterus, and sometimes thickening cervical mucus.
Physicians generally agree that combination pills can protect against a range of conditions both minor and severe, including cancer of the ovaries or lining of the uterus, ectopic pregnancy, excess body hair, iron deficiency anemia from heavy menses, noncancerous breast growths, osteoporosis, ovarian cysts, PMS, and vaginal dryness. According to Planned Parenthood, protection against ovarian and endometrial cancer can last for up to 30 years after stopping use of a combination pill, and protection increases with each year of use. In the short term, combination pills can, however, cause a change in sexual desire, depression, nausea, and vomiting. If these continue beyond three months, a clinician can adjust the prescription accordingly.
The bad news? Women using combination pills have a slightly higher chance of developing blood clots in the legs, lungs, heart or brain, most often following a major surgery or immobilization of a leg through bed rest or a cast. Some women will develop high blood pressure and, though fewer in number, others will develop liver tumors, gallstones, or jaundice. Risk factors include being a smoker over the age of 35, a history of blood clots or heart valve problems, an abnormal growth or cancer of the uterus, history of heart attack or stroke, and history of migraine headaches with aura.
Another "tea party" may be in order these days as concerns that the latest studies on long-term use of the Pill may follow in the footsteps of the controversy surrounding hormone-replacement therapy (HRT). Early studies of HRT found that it decreased the rate of heart disease, only to be overturned by later clinical trials that found the "protection" was a matter of economics, not medicine. But many, if not most, of those studies are of women opting for oral contraceptives and may suffer from a similar socioeconomic bias - the annual physical and monthly prescription are not always covered by insurance, after all. Similarly, many studies of oral contraceptives currently indicate protection against ovarian and endometrial cancer. In fact, last fall The British Medical Journal found that women using oral contraceptives had a 12 percent lower overall risk of cancer.
According to the Mayo Clinic, using birth control pills for longer periods of time may increase a woman's risk for cervical and liver cancer, even while protecting against ovarian and endometrial cancer. A study published in The Lancet last November found that use of oral contraceptives for more than five years was associated with an increased risk of cervical cancer. The same study also found that the risk fades over time after ceasing use of birth control pills, returning to normal after 10 years.
The impact on breast cancer is even less clear, with some earlier studies indicating a link between long-term use of oral contraceptives and breast cancer, and more recent trials disputing those findings. An initial examination of 54 existing studies in 1996, for example, found an increased risk of breast cancer for women currently on the Pill, but a report in The Journal of Obstetrics and Gynecology last year found no correlation between the survival rates among breast cancer patients and current or previous use of oral contraceptives.
In addition, research presented at an American Heart Association meeting last year found a 20 to 30 percent increase in arterial plaque for every 10 years that a woman uses oral contraceptives. For perspective, however, the annual risk of dying for non-smokers using oral contraceptives is just two out of every 100,000 women, according to ARHP, compared with 12 out of 100,000 women at risk of death from pregnancy during the same time period.
The impact of hormonal contraception on cholesterol is even more complex and depends on both the type of pill and level of dosage. Physicians track four measures of cholesterol - low-density lipoprotein (LDL, "bad"), high-density lipoprotein (HDL, "good"), tryiglycerides (lipids or blood fats), and total cholesterol. The estrogen in combination pills causes an increase in HDL and a decrease in LDL, as well as an overall increase in total cholesterol and triglyceride levels. Progestin-only pills have the opposite effect, according to the Mayo Clinic.
Classification and Funding Struggles
The politics of contraception extends beyond the laboratory and physician's office, however, to the role of government agencies and public funding in private reproductive rights. The FDA's foot-dragging on approving non-prescription access to emergency contraception is the most well-known and recent example. It's been led in part by objections of Dr. David Hager, appointed by President Bush to the FDA's Reproductive Health Drugs Advisory Committee despite his denunciation of the Pill, and his recommendations that premenstrual syndrome be treated with prayer. Even condoms are being classified differently (read: politically). New versions of male condoms, for example, need only pass tests for leakage and bursting, while female condoms must pass clinical trials on par with pacemakers, heart valves, and silicone breast implants.
Federal restrictions on the use of funds for reproductive services usually refers to the Hyde Amendment's prohibition on using Medicaid funds for abortions. However, federal funds provided 91 percent of the $4 million spent in Vermont on contraception in 2001 through Title X of the Public Service Act, the only federal program devoted solely to the provision of publicly supported family planning services. And according to the Guttmacher Institute, half of the more than 70,000 women in Vermont who require contraceptive services and supplies need public funding because they are teenagers or have incomes below 250 percent of the federal poverty level.
With 11 percent of American women who do not use contraception accounting for half of all unplanned pregnancies, the link between the cost of contraception, its use, and the rate of American abortions is clear. The most recent data indicates a troubling trend, however. Between 1995 and 2002 contraceptive use fell among all women at risk of unintended pregnancy (defined as women who are sexually active and able to become pregnant, but not seeking a pregnancy), according to a report last year by Guttmacher. The drop in contraceptive use was most severe for women in poverty, however, from 92 to 86 percent. Correspondingly, between 1994 and 2001 the annual decline of unintended pregnancies (and therefore abortions) stalled. At current levels, half of all American women will face an unplanned pregnancy at some point; poor women are also four times as likely to experience an unplanned pregnancy and three times as likely to have an abortion compared with higher income women.
Where Are We Now?
The verdict on the health impacts, good and bad, of long-term oral contraception remains cloudy, and the ongoing use of women's health as a political football makes an objective rendering of data highly unlikely. The dramatic impact of the Pill and its progeny on the rest of women's life, however, is indisputable. The Pill revolutionized modern life by offering women long-term female-centered control of their fertility. It's a legacy important to remember even as we continue to insist that the science privilege the real experiences of women using the various methods above the rhetoric and power struggles of politics as more women in each successive generation spend more total years of their lives opting for synthetic infertility.
Vermont Woman Assistant Editor Mary Fratini lives in Barre. She can be reached at maryfrat@vermontwoman.com
|

