  |
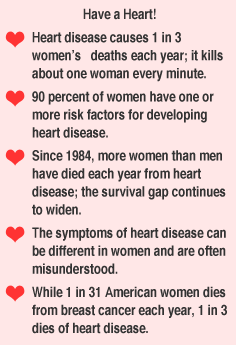
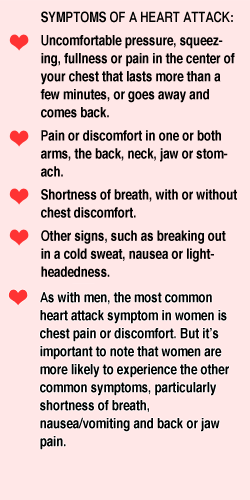
Although heart disease is often thought of as a men's disease, this number-one cause of death in the U.S. kills more women than men each year. The good news is that many of the risk factors are preventable.
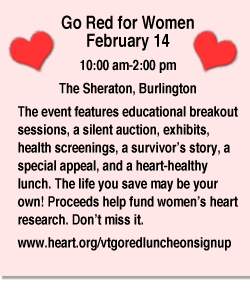
One of the champions of educating women, the American Heart Association, marks its tenth anniversary this year. Its "Go Red for Women" initiative helps more women take charge of their health.
The campaign provides education about women's risk factors, greater awareness of gender-specific heart attack symptoms, and tools to make more healthy lifestyle choices and changes.
Funds raised by Go Red for Women will support educational programs and heart research and treatments focused on women. Some of our risk factors, such as smoking, obesity, elevated LDL cholesterol, and high blood pressure, are familiar to us. Less well known are: estrogen effects, how sleep patterns affect obesity, how sugar consumption translates into blood fats, the relationship between women's abdominal girth and cardiovascular disease, and new terms such as metabolic syndrome. More gender-specific research has already increased the body of knowledge, but more is needed.
Leading Lifestyle Medicine
This year's Vermont Go Red sponsor is Northwestern Medical Center in St. Albans. Its chair is Jill Berry Bowen, who is NMC's CEO. On Valentine's Day, she and others will present at the Go Red for Women event in Burlington. (Sign up below). She will share the results of the hospital's pilot heart-healthy class for women.
The hospital's 12-week program was adapted from the AHA's heart makeover program aimed at lowering cholesterol, blood pressure, and living heart-healthy. The class is being offered as part of NMC's employee wellness program, recently renamed Lifestyle Medicine.
"Wellness is the future," Bowen says about the heart makeover class, and the new name for a hospital department. "Traditional hospitals need to evolve from a place of treatment, to promoting a healthy lifestyle across the community, to being the catalyst. —That's what the community needs—they need leadership."
It is Bowen's goal to have NMC's employees improve their own health first, and become leaders for the greater community. "What about the hospital being a role model?" asks Bowen, whose undergraduate degree is in community health. "If we can limit controllable risk factors, then we are going to impact health. Cardiovascular and other chronic diseases are what come into the hospital. And these are largely built on behaviors and choices that start at a young age."
While Bowen is both a student in the heart-healthy class and its champion, she credits Dr. Elisabeth Fontaine, an obstetrician-gynecologist at NMC, as the force behind it.
Fontaine, a lithe powerhouse of a woman, has long held a vision of teaching people to improve their health via a lifestyle medicine approach. With her own passion for fitness, and an educational background in physical education, obesity and exercise physiology, and genetics, Fontaine saw a golden opportunity when she sat on the Go Red for Women executive committee in 2011. The committee also included Mary Powell, CEO of Green Mountain Power and Go Red chair. Fontaine could bring heart makeovers to NMC. |
Doctoring Changes
Fontaine's interest in a lifestyle approach to wellness was also fueled by her ob-gyn practice. "In some patients, I would notice their blood pressure creeping up," says Fontaine. "I would then send them to their primary doctor, and find they would come back to me, now on a blood pressure medication, and no lifestyle teaching. That is not what I wanted to see."
And while her hospital has for a long time offered health risk assessments to employees, Fontaine always felt there was something missing. "We evaluate people, but what is the step after? What do you offer them? People need education."
The Pilot Class
Fontaine organized an education team, including NMC wellness nurse Pam Cross, personal trainer Monica Pelletier, and herself as a physician resource.
She rallied several of the ob-gyn nurses she worked with to be participants in cycle one of the class. Because she sees these nurses on a regular basis, she was readily available to them as a resource, and she could easily notice changes. |
~American Heart Association |
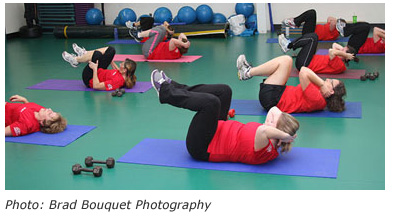
She says she sees "different faces" these days. By Valentine's Day, two classes of employees will have completed 12-week cycles. The class meets twice a week, with an hour-long exercise class on both nights; on one night there was also time for education, questions, and reflection.
Pelletier, who teaches the fitness component, says, "I am excited that we are doing it in a way that gives people the tools for success in lifestyle change. I've watched people in two groups. Most of them hadn't exercised before, and saw it as a chore. When they see they can do it, and see the results, they are encouraged to do more. Now I have people who couldn't do a stomach crunch doing 150, and some people are running who never ran before."
Pelletier exposes them to different types of exercise, such as kickboxing, and Pilates, to let each participant find out what uniquely interests them. Fontaine adds, "We teach them the importance of both aerobics to improve cardiovascular health, and resistance training to improve muscle mass, which helps to burn calories."
|
Inputting Data
Data collection is vital to the program's continued success and to winning future grants and to getting insurance companies to see the benefit of wellness. To that end, at the hospital's expense, the wellness nurse collects blood work including cholesterol and blood sugar levels before and after the 12-weeks cycle. Blood pressure, waist circumference, and body mass indices are recorded at each class.
Food logs and energy expenditures are tracked through a tool called a "Fit Bit®," a device similar to a pedometer and worn on the body. Fontaine follows the participants, who range in age from about 30 to 60, on her computer's "room with a view," she jokes. She views all the data and tracks them, and offers suggestions for improvement where needed.
"I can counsel them about eating habits, and answer anything they may be confused about." The Fit Bit® is just one brand of a type of device that comes with its own software program, and which is designed to break down the daily food intake the wearer records into calories, fats, carbohydrates, proteins and other nutrients—and then calculate the day's energy expenditure via steps or stairs taken.
Additionally, it will track sleep patterns. A growing body of research shows a relationship between sleep deprivation and physiologic changes. These can lead to obesity and diabetes, both risk factors in cardiovascular disease, Fontaine will refer participants to seek further evaluation for any sleep disorders, such as sleep apnea or insomnia.
|
 |
 |
Not About the Pounds
Fontaine emphasizes that "The class is not about weight loss, though that is a happy byproduct. Weight loss is easy," she says, "but, keeping the weight off, and making lifestyle changes is the hard part."
A participant from the first class, Darla Lothian, RN, says, "The biggest changes I have noticed were improvement in my sleep. And when I am eating healthy I am not craving sweets." Lothian says her systolic blood pressure has declined from 130 to 120. The drop in weight she experienced makes her want to keep going.
Over the summer break, when the program ended, her Fit Bit® was taken away. "Even after we stopped using it," Lothian observed, "we knew what we needed to do in a day to spend those calories."
Intentionally or not, Fontaine chose a ideal group to follow, as nurses are prone not only to interrupted sleep cycles, but to eating on the run. "I look at food differently now," says Debby Choquette, RN, another participant. "I know more about the food's value, and ask myself if I want to eat that. I now know the importance of smaller frequent meals with protein, instead of quick re-fuels."
Choquette credits the mentor component of the program as being especially helpful. Fontaine structured it so that cycle-one participants are paired with cycle-two participants. "It's a motivator to have a partner to work out with," says Choquette.
Stephanie Koch O'Brien, RN, and NMC's Family Birth Center's nurse manager found the class fun. For her, the aerobics were easy, but the weights, she said, "push us more. And if I don't make my 10,000 steps a day, I find myself jogging in place to make it up."
Group encouragement proved important to her. Planning to meet someone to walk, or promising another person to walk that morning separately motivated her to exercise.
|
 |
Self-Measured Success
Cassie Gordon, who works as a financial clerical staff, is the eldest class member. At 63, Gordon has a history of arthritis, scoliosis, and asthma. |
Her triumphs included being able to walk longer without stopping to catch her breath, a dramatic drop in her cholesterol, and learning through the Fit Bit® that she was waking up 20 times a night.
"I was discouraged at first," says Gordon, "But I learned to do it at my own pace, and not compete with the girl next to me."
Having the hospital's boss take the class is likely an endorsement in itself. Bowen, a cycle-one participant, says her biggest improvement was lowered cholesterol. "I also eat a bigger breakfast, and drink more water," the busy CEO says. "Sleep is still an issue, and I haven't had a chance to get my sleep assessment yet."
Bowen is enthusiastic about the impact on her employees so far. "When the first group came back from summer break, it was not about how much weight they lost, but they were talking about not having to take their blood pressure and cholesterol pills, and that they were able to sleep, feeling better about life. It's amazing how this was done—not by focusing on weight, but by just living."
Talking Points
An energetic teacher, Fontaine walks through the hospital saying hello to everyone by name, while expounding on her field of expertise, obesity physiology. "Sure, everyone is cutting down on fats, but in the last twenty years, people have become addicted to sugar, and the carbohydrates are now in the 50-60 percent range. That needs to be reduced. And what many people don't know is how carbs feed the triglycerides, and how too much abdominal fat feeds the triglycerides.
"We teach people about the top-ranked DASH (Dashforhealth.com) and Mediterranean diets for controlling blood pressure. Also how the time of day affects calorie expenditure, and how important it is to vary foods you eat."
Fontaine teaches participants not to eat less than 1,200 calories a day, and says studies have shown that if you journal what you eat, you will lose weight and keep it off, owing to a greater understanding of calories.
Fontaine has invited a colleague from Quebec, Dr. Jean-Pierre Deprés, a professor in cardiac research at Laval University and a specialist in cardio-metabolic risk, to speak at the Go Red for Women luncheon. Deprés will present his often cited research on the subject of abdominal obesity, or visceral adiposity, and its relationship to heart disease and metabolic syndrome. Metabolic syndrome is a name for a group of risk factors that occur together, and increase the risk for coronary artery disease, stroke, and Type 2 diabetes.
In an interview posted on YouTube, Deprés encourages primary care doctors to measure both BMI and waist circumference as a screening tool for cardiovascular risk, since BMI alone can be misleading. |
 |
A Growing Trend
Incentivizing wellness is a growing trend in businesses. Because preventable chronic conditions caused missed work, lowered work morale, and increased health care insurance premiums, it just might benefit employers to offer financial incentives to employees to improve their health.
There are legal constraints against discrimination, but this can be avoided by offering many options and presenting choice, not a mandate.
NMC has steadily added incentives to its wellness program; some include spouses and civil union partners. But it was Dr. Fontaine who noticed that only a low percentage of employees participated, that there was no significant improvement in the biannual health risk assessments, and that hospital insurance costs continued to rise.
"We have to ask, what will be the trigger that will prompt change?" said CEO Bowen. "We've tried the fitness center, wellness offerings, healthier food choices in the cafeteria. We tried different things." Some worked, she said, but for others it was a pocketbook issue.
New this year are economic incentivized goals. If 75 percent of NMC employees achieve a BMI of 30 or less—a relatively gentle goal since a BMI greater than 25 is considered overweight and a BMI greater than 30 is considered obese—all employees will be eligible for a portion of the bonus awarded for the year.
When an individual achieves a BMI of less than 30 and also has two health risk appraisals, a preventive health screening, and documents she is tobacco-free or trying to quit, her payment for her health insurance premium will be reduced. To Bowen, this is not just about hospital cost savings.
"We are trying to set the expectation and to role-model the behavior that we want to see in the community—to live better lifestyles that will ultimately result in better health of the population. How do we facilitate that? This hospital has 750 employees. In our strategic plan, we want to tackle obesity in the community. If we can do it here, then we can take it out to the community."
|
To Community—And Beyond
The heart makeover pilot program and data collection are part of a larger plan. Both Bowen and Fontaine envision bringing wellness and lifestyle medicine to the community. They want to illustrate to insurance companies that prevention can impact healthcare costs. They want to teach other businesses and corporations how to care for their employees' wellness and show them why it matters. More data is needed for that.
"The hospital has paid for everything so far— the Fit Bit®, the use of the gym," said Bowen. "We will need grants to bring the program into the community to help people who can't pay. And we need to measure the impact on health, to show what will be the return on investment. Can we take employees and improve their health? What is the impact on health insurance? We will take all of that information, and record statistics. We will need to show numbers to see the impact."
The combined work of the AHA Go Red for Women along with Bowen and Fontaine's Lifestyle Medicine team and its pioneering participants at NMC may lead the way to a new culture of wellness. The next step is widening their community data, and showing other businesses that they, too, can do more than offer health insurance to their employees.
Prevention is, after all, the best health insurance of all.
Roberta Nubile is an RN and an award-winning writer who regularly contributes to Vermont Woman. |
~American Heart Association
|
|