Is There a Doctor in the House? YES, Two! Drs. Karen Hein and Allan Ramsay |
|
| By Roberta Nubile | |
 |
 |
| Dr. Karen Hein and Dr. Allan Ramsay are the two physicians currently serving on the Green Mountain Care Board. Both Ramsay and Hein have formidable credentials and deep commitments to reform. photos: Jan Doerler |
|
| The wool that Dr. Karen Hein gathers from the herd of cashmere goats at her Whitingham, Vermont home has had to wait for her to card, spin, weave, knit, and felt it. Her creative energy, she says, now goes into her work on the Green Mountain Care Board (GMCB) as she heads into her third and final year of service.
Meanwhile, the goats, too, must wait for the days of the week that Hein and her spouse Ralph return home; the rest of the week they stay in Montpelier, to lessen the commute.
Hein says all her life’s work thus far has lined up perfectly for her service on the board. By her own account, she has taken an “unusual journey for a physician,” working in academia, the federal government, foundations, and in global health care where resources are scarce. Hein’s broad background has shaped her lens. She says her personal approach to the work of the board has at times been different from that of other key people at the helm. She says her big-picture approach is both her contribution and, at times, a source of struggle for her. “We have a lot of people looking at the puzzle pieces. And I am always asking, how does this piece fit into the bigger picture? With any new insurance rate review or certificate of need we must approve, I always ask: ‘What is it that we are building, and where are we in that vision?’” From Hein’s point of view, improving Vermont’s health care system is necessary and important. But her goal takes improvement one step further. What really gets her heart beating faster is preventive health and something called “population health,” which by definition looks at the broader and more long-range picture. It takes more time to see a return on investments in these areas. She wants to know how Vermont healthcare reform can keep individuals and populations healthy and prevent them from needing health care. |
|
|
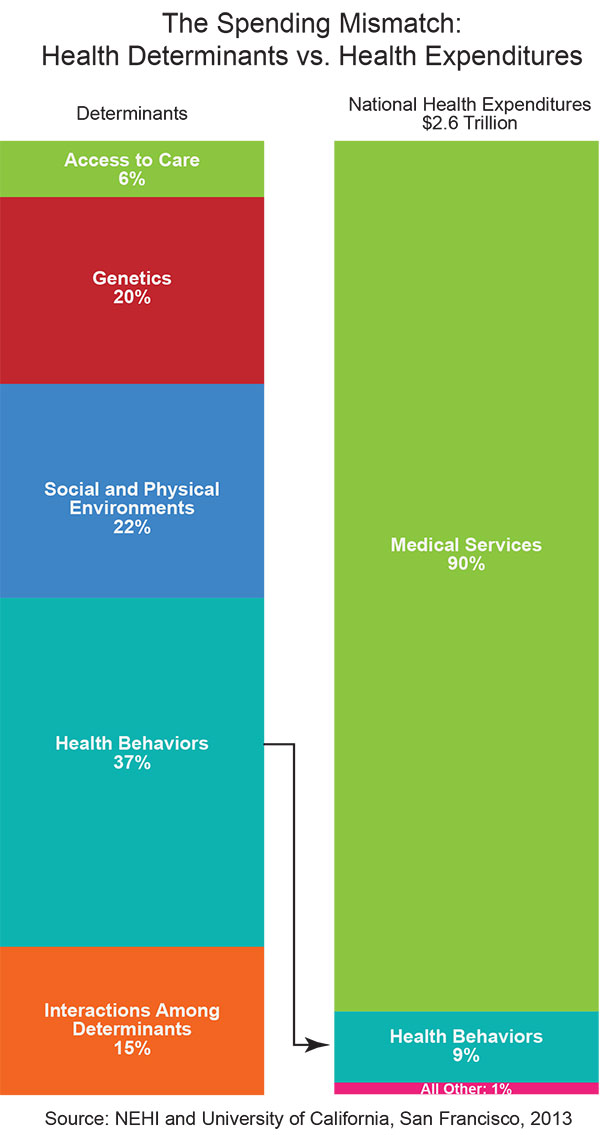
Population health, says Hein, asks a question that the GMCB is mandated to address: How healthy is Vermont’s healthcare system? Hein explains, “Now, if we were to ask what are the actual contributors to health, we call these the social determinants of health. These have been written about in the last 20-plus years, and include things like genetics, behavior, and healthy choices, as well as public health, the environment, and the health care system. “Many studies have been done to look at how big an influence, by percentage, each of these social determinants has on health, or premature mortality (See graph). It turns out, by some estimates, the contribution of health care to overall health is only 10 percent. Yet, we are spending much money on the health care system, roughly 80 percent of every health care dollar. “We are doing good work on the healthcare delivery system part: We do only what is evidence-based; we don’t over treat. But that is just the healthcare piece. Actual health comes mostly from what choices we make: how we eat, exercise, and care for ourselves. Lots of other countries have done far more in the public health and population health arena. “With only three or four cents of Vermont’s healthcare dollar spent on this, I am asking people to turn their attention to evidence-based interventions we know will improve public health. “We have done good work with smoking cessation, for example, so we know we can do it. It’s just that we haven’t done it often. And we haven’t done it much. We have a choice. We can continue to spend just three or four cents on the dollar on prevention, and wait for people to develop diabetes and heart failure and renal failure, and pour all that money into caring for those people. |
Dr. Karen Hein poses in the Goat Spirit mask with her beloved cashmere goats. The mask was made by Tristham Gregg of Haines, Alaska, as part of efforts to bring back storytelling in the Tlinket tradition. This has special meaning since her husband, Ralph (Dell), was born and raised in Alaska. Photo: Joan Waltermire |
“Or, whoa! What if we prevented some people, a few people, from getting those diseases in the first place? So let’s get on with that. That is my goal, my dream, my contribution.” Hein is pleased that a recent federal State Innovation Model award, or SIM grant, includes funds for committee members to attend to population health sessions in Vermont. “This is where you see the integration of population health into each of the activities that we are already doing. Then I think we have a chance with prevention and early intervention. “The return on investment takes longer, 15-20 years, a much longer return than say, payment reform. But that’s where you start to see huge improvements in the cost of health, if you were to implement what is evidence-based in population health.” Why then, if health care systems have so little impact, does GMCB focus on healthcare system reform? Hein replies, “People say it’s a huge ship. Even though health care is not the major contributor to health, it sure is the major drain of resources. My point is, let’s do both.” Hein says what has surprised her most about her work on the board is the lack of obstacles to such a complicated task. “What enables us to make real progress,” says Hein, “is the good will of Vermonters to trust the law and the process.” Of her fellow board members and staff, she says, “Plus, we have a phenomenally talented group of people. In all the sectors I have worked in, I’ve never met such a group of technically skilled, dedicated people and, especially welcome—when things gets tense or hectic—is that some even come with a sense of humor as well!” Hein is also awed by the enormous financial investment it takes to make the necessary changes for a more streamlined system that works. “Hundreds of millions of federal dollars have enabled us to make technical infrastructure changes to allow all the electronic health records to ‘talk’ to each other. We are very data driven. Vermont is one of the first states in the country to have all the payer data—Medicare, Medicaid, and commercial insurers—in one database, which makes our work so much easier.” Hein is referring to the “all-payer claims database,” a relatively new tool that allows policy makers to evaluate utilization, expenditures, and quality of health care. Hein has had personal glimpses into Vermont’s health care system. She has shared in her physician husband’s progression from cognitively impaired to a diagnosis of Alzheimer’s. She feels grateful for adult daycare. Her husband, Dr. Ralph Dell, attends one in Barre, which she says he enjoys for the community it offers him. She also says that while there are 16 such facilities in Vermont, that number is not nearly enough. “I have a deeply meaningful life, which is saturated in color,” Hein says. She spends free time with her and Ralph’s blended family of four children and three grandkids. She unwinds with aerobic sports like running, swimming, and skiing, and enjoys her beloved cashmere goats. “We are all in this together,” she says of her work. “When people think of us—the board—as the regulators and innovators, really, the innovation needs to come from each of us, every Vermonter. We need to ask how we can reinvent ourselves to be healthier people, or all this regulatory stuff isn’t going to work.”
More than once during our interview, Dr. Allan Ramsay, GMCB’s other board member reflected on how much he missed being in the room with his patients as a family doctor. To serve on the Green Mountain Care Board without a conflict of interest, Ramsay knew he would have to regretfully leave his 32-year family medical practice. But when the call came for applicants to Vermont’s Green Mountain Care Board, it was there he saw an opportunity to help protect what he values most: good quality, affordable patient care. “Before I put in my application to be considered for the GMCB,” says Ramsay, “I researched healthcare reform all the way back through Tommy Douglas in Saskatchewan in the early ’50s, up to Vermont’s healthcare reform efforts in the ’90s.” Douglas is credited with establishing Canada’s first single-payer universal healthcare program. “I did the research, because I knew I would be transitioning from something I truly loved, as a doctor in family medicine and palliative care, to a whole different career. It was in doing all that research, I realized—and knowing the views of so many of my provisional colleagues around the state—that Vermont would be a place where we could do it.” Ramsay has a history of seeing what is missing, and doing something about it. As a young doctor, he started a nonprofit rural health clinic to care for underserved populations in Colorado. Valley Wide Health Services is now widely considered a model for rural health care, and is one of the largest in the U.S. After moving to Vermont, practicing here, and teaching family medicine at UVM, he recognized the unmet needs of chronically ill patients who needed symptom management. He helped develop Fletcher Allen Health Care Palliative Care Services and founded the Rural Palliative Care Network. While his distinguished medical and academic career and board work is well documented, what becomes apparent in talking to Ramsay is his passion for direct care of his patients. While serving on the GMCB, he volunteers one day a week as a doctor at the People’s Health and Wellness Clinic in Barre, Vermont. Ramsay says, “It keeps me sane.” Ramsay views himself as a liaison to his fellow healthcare providers in Vermont. He plays a role similar to that of Al Gobeille. The board chair sees himself as a voice for the business community in health care reform (See the most recent in Vermont Woman’s series, Sept/Oct. 2013). Ramsey’s base is medical professionals. “I recognized right from the start,” Ramsey says, “that my constituency—my professional colleagues all around the state—would expect me to keep them informed, to allay their fears, help understand what their concerns were, and make sure they were getting the right message about what we were trying to do.” Primary care doctors like Ramsay are much needed. Dr. Charles MacLean, the associate dean for primary care at the UVM College of Medicine recently told WCAX that although New England’s shortage of primary care doctors is not as severe as in other parts of the country, some estimate that Vermont needs an additional 50 doctors practicing general medicine. Ramsay talks of job satisfaction: “My primary care colleagues fear nothing will change for them in terms of administrative burdens, like prior authorizations for tests. Now we have a tool for developing a pilot project to make that better. What they love is what happens when they are in the examining room with their patients. What they hate is the things that happen at the computer at the end of the day when they are not with their patients.” Since Ramsay joined the board, he has spoken to well over 1,200 of his colleagues throughout the state. He is presently geared up to make another wide-ranging tour to provide updates and information to health care providers about GMCB’s activities. Says Ramsay, “My goal is to help them understand that this is a balance between controlling costs, and doing the right moral and social thing for Vermonters. It means providing high quality healthcare that is accessible and affordable. Every other country that has done this well before us, has [tried to] balance the moral with the financial issues around health care.” One issue not dealt with in Vermont’s Act 48 is malpractice reform. The cost of malpractice insurance is widely thought to have an effect on health care costs. Physicians’ worry about malpractice liability can lead to overuse of diagnostic tests and procedures that contribute to high health care costs. Ramsay says, “I have worked with the Vermont Medical Society to make changes. This is a highly emotional issue that has to be addressed. If you look at the data, Vermonters are not highly litigious, but defensive medicine can lead to waste in the system.”
The past year has challenged Vermont’s hospital CEOs and CFOs as they worked to meet the GMCB-imposed budget cap of 3.75 percent growth for 2013. The aggregate of Vermont’s 14 hospitals’ net increase was 2.7 percent. While the goal was met, the jury is still out as to how exactly that happened. Was it from health care reform innovations to increase efficiency? Was it a decrease in the over-utilization of tests? Or was it the result of a depressed economy and part of the national trend of decreased health care use by consumers? Ramsay says it may have been a combination of factors. He intends to learn more of the story directly from healthcare providers. Ramsay says, “I will hear from my colleagues when I tour around the state whether lower revenues has had any impact on what they perceive to be the high quality care they are already providing. If I hear that, then it won’t be as great a story.” But Ramsay is hopeful. “A certain portion has got to be the fact that healthcare providers are taking this [reform] challenge seriously.”
While a large part of GMCB’s role is to regulate costs for Vermont hospitals and insurance companies, what excites Ramsay most is the opportunity to improve care. “It’s our responsibility to foster innovation throughout the system,” he says. “I get comments all the time from my colleagues as to what they think would make the system work better—and what would make the patient experience better.” A few examples of Vermont’s many innovations include both old and new programs. The Vermont Managed Care and Blueprint for Health has been enveloped by the federal Accountable Care Organizations (ACO). (See The Story Behind All Those Health Acronyms sidebar and Vermont Woman’s article on ACOs in our Feb/March 2013 issue). The smaller of Vermont’s two ACOs is the Accountable Care Coalition of the Green Mountains. Established by HealthFirst and located in South Burlington, it has an all-male board of physicians; it is providing Medicare and Medicaid patients with “enhanced care coordination,” while participating in the federal Shared Savings Program. One of Ramsay’s favorite quality indicators is physician-patient shared decision making, under which the physician gives the patient all the options and evidence around a treatment plan. Ramsay says, “It’s not, ‘I make a decision and you go along with it.’” Another innovation Ramsay feels close to, as a family doctor, is a pilot study at Fletcher Allen Health Care initiated by its third-year medical residents, and based on a national program called Choosing Wisely. The Choosing Wisely program, according to its website, asked more than 30 groups of specialists to come up with “five tests or procedures commonly used in their field, whose necessity should be questioned and discussed.” If that happens, and patient usage goes down, how will hospitals stay afloat economically? Ramsay acknowledges that Vermont is in a period of transition. “How do we move from being paid to provide services to being paid to provide higher value and more efficient, more evidence-based health care? We are in a very difficult transition time. When hospitals see utilization going down in terms of surgery, imaging, lab tests—they have to make it up somehow. They still have those fixed costs.” Ramsay says change won’t come overnight. “To translate that into actual patient care is an evolution.” As an example, Ramsay describes a patient with end-stage renal disease who is on dialysis who may be admitted for other medical or surgical reasons. “The Family Medicine and Surgery departments at Fletcher Allen decided to look at how many times kidney function tests were being ordered on these patients,” says Ramsay. “Now, when you are on dialysis, specific kidney function tests are not very valuable, because you are being dialyzed every other day. But, they were being ordered. “Just that simple elimination of a blood test not only improved patient experience—to not be awakened at 4:00 a.m. for the test—but it reduced cost of care as well. Just in the pilot project alone, over $100,000 was saved. When you see things like that developing spontaneously, you have to be optimistic. After a year and a half into this process,” Ramsay laughs, “I am still an optimist. I believe we can do things in Vermont that haven’t been done anywhere else.” Of his time on the board, Ramsay says, “My learning curve has been very steep, and continues to be so. We have a great staff and smart people. The GMCB functions well. We learn from each other, and respect each other’s opinions. The main thing I have learned is how difficult change is, and how threatening it can be.” When Ramsay’s term ends in 2016, he says he’s not sure whether he will return to direct patient care. But he is sure he will continue to do healthcare community work. Ramsay maintains his personal well-being by running, playing golf, and visiting with his three grown children. He reports that his wife, Ann, a registered nurse and a traditional Chinese medicine practitioner, convinces him to keep his “yin and yang in balance.” He says, “We do have some interesting discussions about health care.” |
|
|
|
|
Roberta Nubile of Shelburne is a registered nurse who has interviewed all the founding members of Vermont’s Green Mountain Care Board. She is a frequent contributor to Vermont Woman. Look for our next issue in early February and her in-depth interview with the first nurse ever to be appointed to GMCB.
|