| Breast Implants: How Safe Are They? | ||
| by Elayne Clift | ||
Largely influenced by pop culture icons suggesting her breasts were inadequate, Denee Dimiceli felt unhappy about the size of her breasts. At age 27, she opted for breast augmentation, despite her spouse’s reassurances that her breasts were fine. Dimiceli’s decision isn’t surprising. Ads promoting breast augmentation abound. “Envision Your New Breasts!” “Fast Breast Enlargement!” promotions boast. Such ads are proliferating and aimed at younger audiences who are choosing augmentation at increasing rates. Wendi Myers had a different experience than Dimiceli. She wanted to remove her implants. Having suffered unexplained dizziness, hair loss, and fatigue, she believed her silicone implants were to blame. When Myers’s implants were removed, she was shocked by the gelatinous material that was excised. Dimiceli and Myers are featured, with plastic surgeons and family members, in a film by Carol Cianutti called Absolutely Safe. Cianutti’s mother suffered from the effects of silicone implants, but the film is open minded, apolitical, and deeply important. |
 |
|
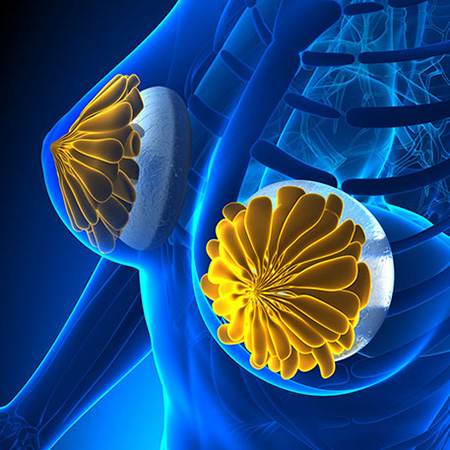
Another 100,000 breast cancer patients had postmastectomy reconstruction, often using implants. According to the 2013 Plastic Surgery Statistics Report, breast implants were the most common cosmetic surgery among women ages 20 to 29, with more than 83,600 procedures done that year. Breast implants made with silicone or saline were first sold in the US in the 1960s. By 1990, almost a million women had undergone breast implant surgery, although no safety studies had been published. The FDA did not require companies selling silicone implants to prove their implants were safe until 1991—after they had been used for nearly 30 years. With increasing problems reported, the media began exposing implant problems and concerns among physicians. Even when safety data were provided to the FDA, they were judged inadequate to warrant FDA approval. In 2000, the FDA required implant manufacturers to prove their saline implants were safe. Silicone gel implants were first approved in 2006 with restrictions, including that women must be older than 22 to receive them.
In 2011, two manufacturers were conditionally approved by the FDA to produce silicone implants in the US. The two companies were required to conduct 10-year studies on more than 40,000 women with implants. According to the National Center for Health Research (NCHR), one of the companies, Mentor, did such a poor job that consumers and public health experts called for the FDA to rescind its approval of Mentor to make silicone implants. The other company, Allergan, lost track of nearly half its augmentation patients within the first two years. The dropout rate of patients participating in studies raises important questions. Did patients stop seeing their doctors because the implants were removed? Were they so happy with implants and so problem-free they no longer wanted to participate in studies? Were they too sick to comply? “Patients tell [us] that plastic surgeons are enthusiastic about staying in touch with patients who are satisfied, but not with patients who have problems,” NCHR reports. One problem with the studies was that they failed to include questions about complications with leaking implants, although women were reporting to the FDA that they suffered from joint pain, hair and memory loss, and other autoimmune symptoms.
Newer research conducted by Allergan followed 455 augmentation patients with first-time implants for at least eight years. Within four years, 24 percent had undergone further surgery to repair an implant problem. One in 10 patients had at least one implant removed. Common complications included loss of nipple sensation, breast pain, and swelling.
|
||
|
The authors of a comprehensive review, “Facts About Breast Implants,” posted by Our Bodies, Ourselves in July 2014, spelled out known risks and problems associated with implants. These problems can be localized within the breast and can include infection, chronic pain, numbness, or breakage and leakage. Scar tissue may form around an implant causing breasts to become hard or tight around the implant. Studies conducted by implant manufacturers showed that within three years approximately three out of four reconstruction (breast cancer) patients and almost half of first-time augmentation patients using either saline implants or silicone gel implants experienced at least one local complication. Longer-term concerns are also worrisome. Bacteria or mold can grow in saline implants, which researchers fear may be released into the body if an implant breaks. The effects of this on women, or nursing babies, have yet to be studied. Other complications of implant breakage involve silicone migration to lymph nodes and other organs. Migration is still not fully understood, but it is raising increasing concerns among researchers and health advocates. As Judy Norsigian, executive director of Our Bodies, Ourselves, has noted, “One of our challenges is helping the public understand that absence of evidence of harm is not the same as proof of safety. Many people assume breast implants are safe because the FDA allows them to be marketed.” Karuna Jaggar, executive director of Breast Cancer Action, an activist watchdog organization, agrees. “There’s a shortage of information about the safety of breast implants that limits women’s ability to make truly informed decisions. With any procedure, it’s always important to balance risks and benefits, but an industry that stands to benefit all too often minimizes risk.” Evidence is mounting that breast implants can make women sick. Some studies suggest that they may be linked to autoimmune diseases such as fibromyalgia. One study found that autoimmune symptoms, including fatigue and joint pain, improved measurably in the majority of women studied who had their implants removed. Another concern is that implants can interfere with detecting breast cancer. An estimated 55 percent of breast tumors remain hidden in women with implants, and FDA reports indicate that because of the frequency of ruptured implants, women may forego mammograms. Further, the accuracy of mammograms tends to decrease as the size of the implants increase in proportion to the size of the woman’s natural breast. Silicone implants usually last between seven and 12 years. Each replacement adds to the cost. Women with silicone implants are advised to have a breast MRI three years after receiving an implant and biannually after that to test for ruptures or leaks. These MRIs cost about $2,000. If silicone implants rupture, they must be removed, adding an additional $5,000 to $10,000. (Saline implants don’t require MRIs and are less costly to remove.) Because these surgeries are considered |
|
cosmetic, they are unlikely to be covered by health insurance. Our Bodies Ourselves and the NCHR are currently working together to ensure that health insurance policies cover treatment and implant removal when medically necessary. Noting that we now live in a “body-changing culture,” Marge Berer, editor of Reproductive Health Matters in the UK, wrote in a 2010 editorial that “in the past 10 to 15 years, there has been a seismic shift in what is considered possible and desirable to change as regards the bodies we are born with.... Surgery has now entered the beauty industry. Women are of course the prime targets of this industry.”
It’s worrying that younger women are being targeted by this industry, especially in the absence of sound data regarding the safety of implants. All women need to know the facts about augmentation surgeries and other cosmetic procedures. As Karuna Jaggar puts it, “We must assert the precautionary principle. We can’t assume that chemicals or treatments are safe without sufficient data to be certain of that.”
|
||
|
Elayne Clift, MA, writes about women, health, politics, and social issues from Saxtons River, Vermont. She has worked internationally as a health communication and gender specialist. Her latest book, with Christine Morton, is Birth Ambassadors: Doulas and the Re-emergence of Woman-Supported Birth in America (Praeclarus Press, 2014).
|
|